Bager, F., 2000, ‘DANMAP: monitoring antimicrobial resistance in Denmark’, International Journal of Antimicrobial Agents 14(4), pp. 271-274 (DOI: 10.1016/S0924-8579(00)00135-7).
Bengtsson-Palme, J., et al., 2018, ‘Environmental factors influencing the development and spread of antibiotic resistance’, FEMS Microbiology Reviews 42(1), p. fux053 (DOI: 10.1093/femsre/fux053).
CMVP and BIOHAZ, et al., 2017, ‘EMA and EFSA Joint Scientific Opinion on measures to reduce the need to use antimicrobial agents in animal husbandry in the European Union, and the resulting impacts on food safety (RONAFA)’, EFSA Journal 15(1), p. e04666 (DOI: 10.2903/j.efsa.2017.4666).
CVMP, 2021, Reflection paper on antimicrobial resistance in the environment: considerations for current and future risk assessment of veterinary medicinal products, No EMA/CVMP/ERA/632109/2014, European Medicines Agency (https://www.ema.europa.eu/en/documents/scientific-guideline/reflection-paper-antimicrobial-resistance-environment-considerations-current-and-future-risk-assessment-veterinary-medicinal-products-first-version_en.pdf) accessed 23 February 2024.
CVMP, 2023, Committee for Veterinary Medicinal Products (CVMP) Work Plan 2024, European Medicines Agency.
DAFC, 2023, Statistics 2022. Pigmeat, Danish Agriculture & Food Council (https://lf.dk/media/onyfd23u/lf-grise-2022-engelsk.pdf) accessed 25 March 2024.
DANMAP, 2023, DANMAP 2022. Use of antimicrobial agents and occurrence of antimicrobial resistance in bacteria from food animals, food and humans in Denmark (https://www.danmap.org/reports/2022) accessed 25 March 2024.
D’Costa, V. M., et al., 2011, ‘Antibiotic resistance is ancient’, Nature 477(7365), pp. 457-461 (DOI: 10.1038/nature10388).
EC, 2018, Options for a strategic approach to pharmaceuticals in the environment, Publications Office of the European Union, Luxembourg (https://op.europa.eu/en/publication-detail/-/publication/5371e7bd-25db-11e9-8d04-01aa75ed71a1/language-en) accessed 26 February 2024.
EC, 2021, EU Agricultural Outlook For Markets, Income and Environment, 2021-2031, European Commission DG Agriculture and Rural Development, Brussels.
EC, 2022, Facts and figures on the common fisheries policy: basic statistical data : 2022, Publications Office of the European Union, LU.
EC, 2023a, EU agricultural outlook 2023-2035, Publications Office, LU.
EC, 2023b, Result indicators (https://agriculture.ec.europa.eu/system/files/2023-09/pmef-result-indicators_en.pdf) accessed 28 February 2024.
ECDC, 2022, Assessing the health burden of infections with antibiotic-resistant bacteria in the EU/EEA, 2016-2020, European Centre for Disease Prevention and Control, Stockholm (https://www.ecdc.europa.eu/en/publications-data/health-burden-infections-antibiotic-resistant-bacteria-2016-2020) accessed 7 February 2024.
ECDC, et al., 2024, ‘Antimicrobial consumption and resistance in bacteria from humans and food-producing animals. Fourth joint inter-agency report on integrated analysis of antimicrobial agent consumption and occurrence of antimicrobial resistance in bacteria from humans and food-producing animals in the EU/EEA. JIACRA IV – 2019−2021’, EFSA Journal22, p. e8589 (DOI: https://doi.org/10.2903/j.efsa.2024.8589).
EEA, 2019, The European environment — state and outlook 2020: knowledge for transition to a sustainable Europe, SOER, European Environment Agency (https://www.eea.europa.eu/soer/publications/soer-2020) accessed 15 April 2024.
EEA, 2022a, ‘Rethinking agriculture’ (https://www.eea.europa.eu/publications/rethinking-agriculture) accessed 1 December 2022.
EEA, 2022b, Zero pollution monitoring assessment, EEA Web Report No 03/2022, European Environment Agency (https://www.eea.europa.eu/publications/zero-pollution) accessed 8 December 2022.
EFSA, et al., 2020, ‘Climate change as a driver of emerging risks for food and feed safety, plant, animal health and nutritional quality’, EFSA Supporting Publications 17(6) (DOI: 10.2903/sp.efsa.2020.EN-1881).
EFSA, et al., 2024, ‘Report for 2022 on the results from the monitoring of veterinary medicinal product residues and other substances in live animals and animal products’, EFSA Supporting Publications 21(3), p. 8669E (DOI: 10.2903/sp.efsa.2024.EN-8669).
EFSA and ECDC, 2024, ‘The European Union summary report on antimicrobial resistance in zoonotic and indicator bacteria from humans, animals and food in 2021–2022’, EFSA Journal 22(2) (DOI: 10.2903/j.efsa.2024.8583).
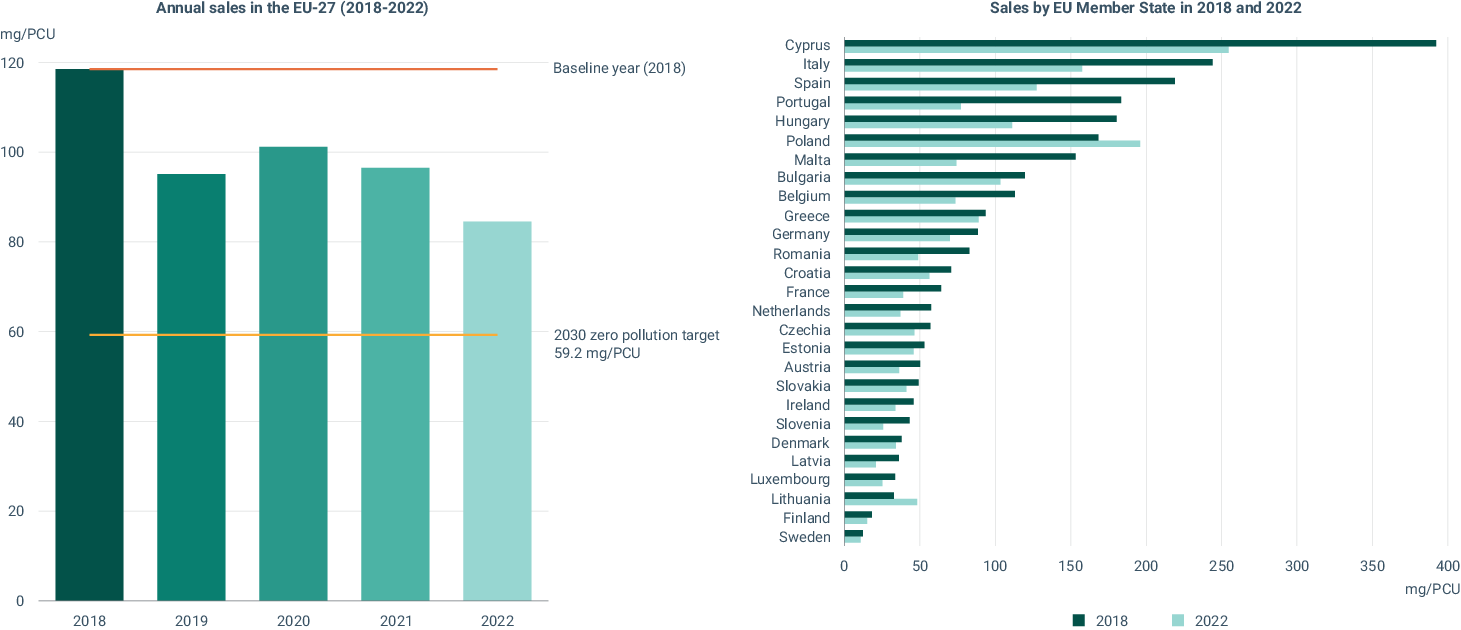
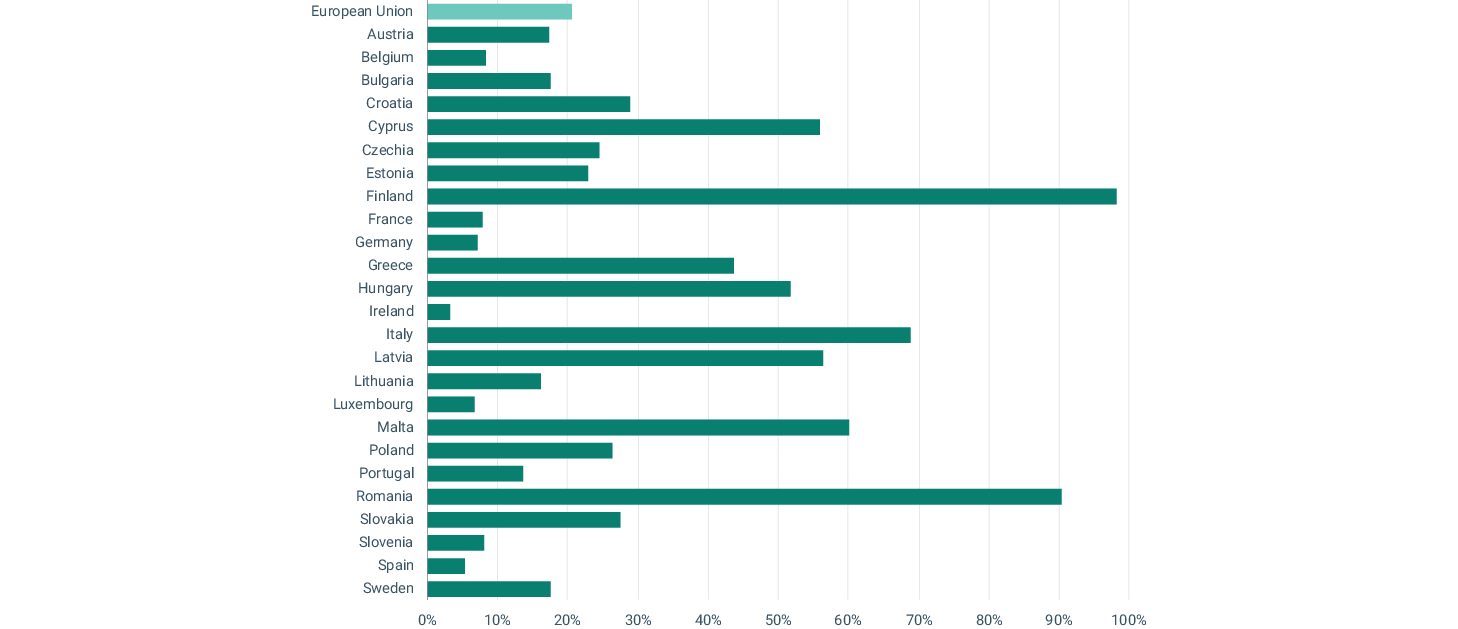
EMA, 2023, Sales of veterinary antimicrobial agents in 31 European countries in 2022. Trends from 2010 to 2022. Thirteenth ESVAC report, No (EMA/299538/2023), Publications Office of the European Union, Luxembourg (https://www.ema.europa.eu/en/documents/report/sales-veterinary-antimicrobial-agents-31-european-countries-2022-trends-2010-2022-thirteenth-esvac-report_en.pdf) accessed 5 February 2024.
EMA, 2024, ‘European database of sales of veterinary antimicrobials agents’ (https://esvacbi.ema.europa.eu/analytics/saw.dll?PortalPages) accessed 27 March 2024.
Eurostat, 2022a, ‘Agricultural production - livestock and meat’ (https://ec.europa.eu/eurostat/statistics-explained/index.php?title=Agricultural_production_-_livestock_and_meat) accessed 5 April 2023.
Eurostat, 2022b, ‘Extra-EU trade in agricultural goods’, Eurostat Statistics Explained (https://ec.europa.eu/eurostat/statistics-explained/index.php?title=Extra-EU_trade_in_agricultural_goods) accessed 14 March 2023.
FAO, 2020,Climate change: Unpacking the burden on food safety, Food and Agriculture Organization, Rome.
FAO, 2022, The State of World Fisheries and Aquaculture 2022. Towards Blue Transformation, General Fisheries Commission for the Mediterranean.
FAO, 2023, The impact of veterinary drug residues on the gut microbiome and human health, FAO.
FAO and FVST, 2019, Tackling antimicrobial use and resistance in pig production: lessons learned in Denmark, FAO, Rome, Italy.
Grenni, P., et al., 2018, ‘Ecological effects of antibiotics on natural ecosystems: A review’, Microchemical Journal 136, pp. 25-39 (DOI: 10.1016/j.microc.2017.02.006).
He, Y., et al., 2020, ‘Antibiotic resistance genes from livestock waste: occurrence, dissemination, and treatment’, npj Clean Water 3(1), pp. 1-11 (DOI: 10.1038/s41545-020-0051-0).
Isidori, M., et al., 2005, ‘Toxic and genotoxic evaluation of six antibiotics on non-target organisms’, Science of The Total Environment 346(1), pp. 87-98 (DOI: 10.1016/j.scitotenv.2004.11.017).
Jechalke, S., et al., 2014, ‘Fate and effects of veterinary antibiotics in soil’, Trends in Microbiology 22(9), pp. 536-545 (DOI: 10.1016/j.tim.2014.05.005).
Jensen, H. H. and Hayes, D. J., 2014, ‘Impact of Denmark’s ban on antimicrobials for growth promotion’, Current Opinion in Microbiology 19, pp. 30-36 (DOI: 10.1016/j.mib.2014.05.020).
Jensen, V. F., et al., 2004, ‘Veterinary antimicrobial-usage statistics based on standardized measures of dosage’, Preventive Veterinary Medicine 64(2), pp. 201-215 (DOI: 10.1016/j.prevetmed.2004.04.001).
Kemper, N., 2008, ‘Veterinary antibiotics in the aquatic and terrestrial environment’, 8, pp. 1-13.
Kirchhelle, C., 2018, ‘Pharming animals: a global history of antibiotics in food production (1935–2017)’, Palgrave Communications 4(1), pp. 1-13 (DOI: 10.1057/s41599-018-0152-2).
Larsson, D. G. J., 2014, ‘Pollution from drug manufacturing: review and perspectives’, Philosophical Transactions of the Royal Society B: Biological Sciences 369(1656), p. 20130571 (DOI: 10.1098/rstb.2013.0571).
Lettieri, T., et al., 2018,State of the art on the contribution of water to antimicrobial resistance.,.
Löffler, P., et al., 2023, ‘Antimicrobial Transformation Products in the Aquatic Environment: Global Occurrence, Ecotoxicological Risks, and Potential of Antibiotic Resistance’, Environmental Science & Technology 57(26), pp. 9474-9494 (DOI: 10.1021/acs.est.2c09854).
Lopes Antunes, A. C. and Jensen, V. F., 2020, ‘Close to a Decade of Decrease in Antimicrobial Usage in Danish Pig Production–Evaluating the Effect of the Yellow Card Scheme’, Frontiers in Veterinary Science 7 (DOI: 10.3389/fvets.2020.00109).
Manaia, C. M., et al., 2018, ‘Antibiotic resistance in wastewater treatment plants: Tackling the black box’, Environment International 115, pp. 312-324 (DOI: 10.1016/j.envint.2018.03.044).
Marinov, D. and Lettieri, 2020, Results of the Watch List under the Water Framework Directive from the 4th reporting year and the combined dataset., Joint Research Centre (https://circabc.europa.eu/ui/group/9ab5926d-bed4-4322-9aa7-9964bbe8312d/library/deabbcb4-c001-4855-b503-04f27996ca7d/details) accessed 26 February 2024.
Markotter, W., et al., 2023, ‘Prevention of zoonotic spillover: From relying on response to reducing the risk at source’, , p. e1011504.
Miller, S. A., et al., 2022, ‘Antimicrobial Use and Resistance in Plant Agriculture: A One Health Perspective’, Agriculture 12(2), p. 289 (DOI: 10.3390/agriculture12020289).
Mulchandani, R., et al., 2023, ‘Global trends in antimicrobial use in food-producing animals: 2020 to 2030’, PLOS Global Public Health 3(2), p. e0001305 (DOI: 10.1371/journal.pgph.0001305).
Munita, J. M. and Arias, C. A., 2016, ‘Mechanisms of Antibiotic Resistance’, Microbiology Spectrum 4(2), p. 10.1128/microbiolspec.vmbf-0016-2015 (DOI: 10.1128/microbiolspec.vmbf-0016-2015).
OECD, 2019, Pharmaceutical Residues in Freshwater : Hazards and Policy Responses, OECD Studies on Water, OECD, Paris (https://www.oecd-ilibrary.org/environment/pharmaceutical-residues-in-freshwater_c936f42d-en) accessed 28 February 2024.
OECD, 2023, Tackling antimicrobial resistance in One Health framework: Policy approaches, OECD, Paris (https://www.oecd-ilibrary.org/social-issues-migration-health/embracing-a-one-health-framework-to-fight-antimicrobial-resistance_34abda8a-en;jsessionid=xYpwYCeAekvDEUf6UXl6P6fGp0q-0O83n1zDoOzR.ip-10-240-5-112) accessed 5 March 2024.
OECD, 2024, ‘Aquaculture production (indicator)’, OECD (http://data.oecd.org/fish/aquaculture-production.htm) accessed 19 February 2024.
OECD and FAO, 2023, OECD-FAO Agricultural Outlook 2023-2032, Organisation for Economic Co-operation and Development, Paris (https://www.oecd-ilibrary.org/agriculture-and-food/oecd-fao-agricultural-outlook-2023-2032_08801ab7-en) accessed 18 March 2024.
OHHLEP, et al., 2022, ‘One Health: A new definition for a sustainable and healthy future’, PLOS Pathogens 18(6), p. e1010537 (DOI: 10.1371/journal.ppat.1010537).
O’Neill, J., 2016, Tackling drug-resistant infections globally: final report and recommendations, Report, The Review on Antimicrobial Resistance (https://apo.org.au/node/63983) accessed 6 February 2024.
Roose-Amsaleg, C. and Laverman, A. M., 2016, ‘Do antibiotics have environmental side-effects? Impact of synthetic antibiotics on biogeochemical processes’, Environmental Science and Pollution Research 23(5), pp. 4000-4012 (DOI: 10.1007/s11356-015-4943-3).
Sarmah, A. K., et al., 2006, ‘A global perspective on the use, sales, exposure pathways, occurrence, fate and effects of veterinary antibiotics (VAs) in the environment’, Chemosphere 65(5), pp. 725-759 (DOI: 10.1016/j.chemosphere.2006.03.026).
Schar, D., et al., 2020, ‘Global trends in antimicrobial use in aquaculture’, Scientific Reports 10(1), p. 21878 (DOI: 10.1038/s41598-020-78849-3).
Statistics Denmark, 2024, ‘Farms with livestock’ (https://www.dst.dk/en/Statistik/emner/erhvervsliv/landbrug-gartneri-og-skovbrug/landbrug-med-dyr) accessed 25 March 2024.
UBA, 2019, The database ‘Pharmaceuticals in the Environment’ - Update and new analysis (https://www.umweltbundesamt.de/sites/default/files/medien/1410/publikationen/2019-06-24_texte_67-2019_database_pharmaceuticals-environment_0.pdf) accessed 22 April 2024.
UNEP, 2023, Bracing for Superbugs: Strengthening environmental action in the One Health response to antimicrobial resistance, United Nations Environment Programme (http://www.unep.org/resources/superbugs/environmental-action) accessed 24 April 2024.
Van Boeckel, T. P., et al., 2017, ‘Reducing antimicrobial use in food animals’, Science 357(6358), pp. 1350-1352 (DOI: 10.1126/science.aao1495).
WHO, 2022, A health perspective on the role of the environment in One Health, WHO Regional Office for Europe (https://iris.who.int/bitstream/handle/10665/354574/WHO-EURO-2022-5290-45054-64214-eng.pdf?sequence=1) accessed 29 February 2024.
WHO, 2023, ‘Antimicrobial resistance’ (https://www.who.int/news-room/fact-sheets/detail/antimicrobial-resistance) accessed 6 February 2024.
Willett, W., et al., 2019, ‘Food in the Anthropocene: the EAT-Lancet Commission on healthy diets from sustainable food systems’, The Lancet 393(10170), pp. 447-492 (DOI: 10.1016/S0140-6736(18)31788-4).
WOAH, 2023, Seventh Annual Report on Antimicrobial Agents Intended for Use in Animals, World Organization for Animal Health (https://www.woah.org/en/document/seventh-annual-report-on-antimicrobial-agents-intended-for-use-in-animals-2/) accessed 19 February 2024.


Document Actions
Share with others